What is MIPS?
The Centers for Medicare & Medicaid Services (CMS) rewards (or penalizes) clinicians or groups who see Medicare Part B beneficiaries based on quality of care, cost efficiency, and patient outcomes. CMS does this through their payment incentive program known as the Quality Payment Program (QPP).
The Merit-based Incentive Payment System (MIPS) is the more common reporting path of two reporting options offered to clinicians and groups under the QPP.
MIPS is the new comprehensive reporting standard that combines elements of and replaces the Physician Quality Reporting System (PQRS), the Value-Based Payment Modifier (VBM), and the Medicare Electronic Health Records Incentive Program for Eligible Clinicians.
Who must participate in MIPS?
If you are one of the following clinician types:
- Physicians (including doctors of medicine, doctors of osteopathy, osteopathic practitioners, doctors of dental surgery, doctors of dental medicine, doctors of podiatric medicine, doctors of optometry, and chiropractors)
- Physician assistants
- Nurse practitioners
- Clinical nurse specialists
- Certified registered nurse anesthetists
- Physical therapists
- Occupational therapists
- Speech-language pathologists
- Audiologists
- Registered dietitians
- Nutritional professionals
- Clinical psychologists
- clinical social workers
- certified nurse-midwives
- Groups or Virtual groups that include more than one of the clinician types above
AND
You meet or exceed the following participation thresholds related to the volume of charges, beneficiaries, and services:
- Clinicians or groups with annual Medicare Part B allowed charges over $90,000
AND - See more than 200 Medicare Part B beneficiaries from October 2024 through September 2025
AND - Provide more than 200 covered professional services to Medicare Part B patients
How does MIPS work?
Your final score, which determines your payment adjustment, is made up of four performance categories, each with their own weight:
1. Quality
This category is about the quality of care you and/or your group delivers to your patients. This category replaces the Physician Quality Reporting System (PQRS).
Most participants will report at least 6 quality measures, including an outcome measure. There are more than 270 possible measures in this category.
2. Promoting Interoperability (PI)
This category promotes both patient engagement and the productive use of the healthcare information you create utilizing certified electronic health record technology (CEHRT). For 2025, Certified EHR Technology use is required for this category unless you are approved for a hardship exemption. This category replaces the Medicare EHR Incentive Program, also referred to as Meaningful Use and was formerly known in 2017 MIPS as Advancing Care Information (ACI).
There is now only one set of measures for submitting data for this category:
- Promoting Interoperability Objectives and Measures
You will need to report on all required measures from each of the 4 objectives, unless an exclusion is claimed, in order to earn any points in the Promoting Interoperability performance category.
In addition, the following attestations are also required to earn a Promoting Interoperability performance category score:
- Security Risk Analysis in 2025
- Prevention of Information Blocking
- ONC Direct Review
Bonus points are available for this category.
- 2015 Edition CEHRT must be used when reporting Promoting Interoperability in 2025.
We review your data for compliance, suggest optimizations, and can help you with earning bonus points for extra measure reporting.
3. Improvement Activities (IA)
This category shows CMS activities you’ve undertaken to improve your care processes, patient engagement, and increase access to your care.
Most participants will attest to completing up to 4 activities during the course of a calendar year. Depending on your practice type, you may be eligible for full credit for this category automatically.
We review your data for compliance and make sure that the IAs you’ve chosen are compatible with QPP’s requirements for this category.
4. Cost
This category is calculated by CMS based on your Medicare claims over the course of the calendar year. This category replaces the Value Based Modifier (VBM). 2018 was the first year this category counted towards your MIPS final score.
Penalties
At a federal level, MIPS must be budget-neutral, meaning all of the incentives must be covered by penalties. Thus, if your organization does not successfully implement a MIPS strategy, the penalties you incur may be distributed as bonuses to competitors.
Penalty adjustments grow by the year as follows:
- Performance year 2017 / Payment year 2019 – 4%
- Performance year 2018 / Payment year 2020 – 5%
- Performance year 2019 / Payment year 2021 – 7%
- Performance year 2020 / Payment year 2022 and after – 9%
Penalties or incentives are applied two years after the performance year for which they are incurred.
Individual, Group, Subgroup & Virtual Group Reporting
Participants in MIPS may report as individuals or as a member of a group.
Individual
If you report MIPS data in as an individual, your payment adjustment will be based only on your performance. An individual is defined as a single NPI tied to a single TIN.
Group
If you report MIPS data with a group, your payment adjustment is based on the group’s performance. A group is defined as a set of clinicians – identified by their National Provider Identifier (NPI) sharing a common Taxpayer Identification Number (TIN), no matter the specialty or practice site.
Subgroup
A subgroup is a subset of clinicians in a group (at least 2 clinicians) which contains at least one individually eligible MIPS eligible clinician. Subgroup participation is only available for reporting a MIPS Value Pathway (MVP) and requires advance registration. Subgroups can’t report traditional MIPS or the APP..
To be eligible to submit as a Subgroup registration must occur by June 30 of the performance year .
Virtual Group
A Virtual Group is a combination of two or more Taxpayer Identification Numbers (TINs) made up of solo practitioners and groups of 10 or fewer eligible clinicians who come together “virtually” (no matter specialty or location) to participate in MIPS for a performance period of a year.
To be eligible to submit as a Virtual Group all groups need have received CMS approval prior to close of business on December 31 of the prior year.
What is the MIPS reporting deadline?
The MIPS Performance Year follows a standard calendar year starting on January 1 and ending on December 31. MIPS participants must submit their calendar year’s worth of data by March 31 of the following calendar year.
How do I get started?
- Click on the blue Sign Up button on the top of the page
- For Individual Clinicians and Groups of less than 10
- Click on Sign up for 2025 under Performance Edition and complete the Registration fields.
- You will immediately receive an emailed link to confirm your email address.
- Click the link to Login with your Username and Password to purchase full access.
- Click on the green Purchase Full Access button at the top of the page and complete the required fields.
- Click on Sign up for 2025 under Performance Edition and complete the Registration fields.
- For Clinician Groups of 10 or more
- Click on Contact Us and complete the form. We will respond to your request within one business day.
MIPS Score Comparisons
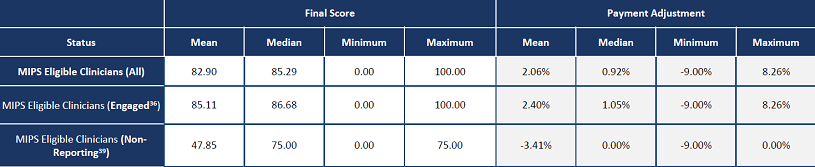
The graphic below shows that on average the difference between reporting and not reporting is 5.81% in payment adjustments. This data is from the 2022 program year which is the most recent CMS data available.